
Choose a channel
Check out the different Progress in Mind content channels.

Progress in Mind
Teaching the patient about their brain can truly make a difference in their engagement with clinicians and with treatment. This improves the chances of successfully managing migraines, said Dr Patricia Pozo Rosich of Vall d’Hebron University Hospital, Barcelona, Spain, at the World Congress of Neurology 2019.
Patients want to know how the brain works and what causes their migraines. This is an important aspect of treatment and empowers them to take an active role.
Patients want to know how the brain works and what causes their migraines
They may have been referred to a headache specialist after several unsuccessful attempts at treatment. Typically in this setting, patients have a high burden from their migraines, which they have suffered from for most of their adult lives. This combination can lead to frustration, hopelessness, and lack of trust. On top of this, there are broader issues such as medication overuse and healthcare costs. So it is important to treat all migraine attacks and prevent them.1, 2
Structural and chemical changes
In a healthy subject, the brain is able to habituate to a headache. But during a migraine attack the brain loses the ability to habituate. This can happen in cycles, leading to episodic migraine, or constantly, causing chronic migraine.3
Neuroimaging reveals differences in the brain anatomy between episodic and chronic migraine. This is evident in cortical surface area and thickness4, in the hypothalamus,5 and in iron deposits.6
The shorter the history of migraine, the more likely a treatment will be effective
Changes in molecular biomarkers of inflammation in the periphery are also associated with chronic migraine.7 In women with episodic migraine, there is a slight increase in levels of calcitonin gene-related peptide (CGRP), and a further increase in CGRP in chronic migraine.8
Chronic migraine also has a characteristic epigenetic profile that research has started to identify. In a rat model, DNA methylation changed most in rats in a chronic migraine state.9 An mRNA expression analysis in human subjects showed that in chronic migraine, pro-inflammatory genes in the periosteum are activated and genes suppressing inflammation are deactivated.10 In another study, microRNA expression also differed between patients with chronic migraine and those with episodic migraine.
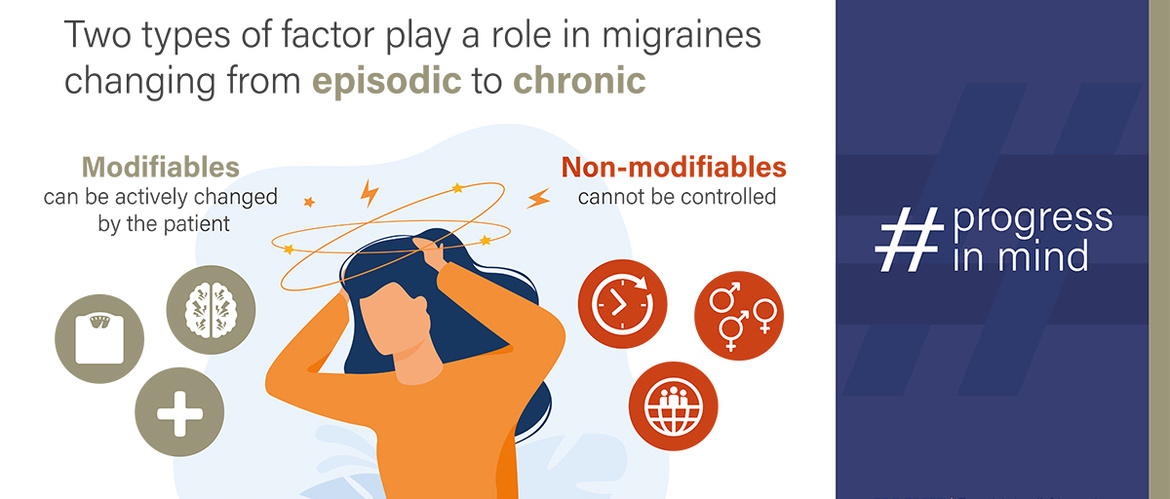
Chronification: modifiables and non-modifiables
When it comes to the change from episodic to chronic migraine, there are factors that can be actively changed by the patient (‘modifiables’) and factors that cannot be controlled (‘non-modifiables’). Modifiables include stress, obesity, and analgesic overuse. Examples of non-modifiables include age, sex, and race.11
A significant modifiable clinical impact factor is how long a patient has been suffering from migraine before been treated. The shorter the history of migraine, the more likely a treatment will be effective. This emphasizes the importance of time to diagnosis and treatment of migraine.
What do patients want to know?
Migraine patients want to find out about their brain and why they suffer migraines. These concepts can be presented to patients.
The lack of habituation is a key concept for patients to understand
Dr Pozo Rosich gave examples of what her patients want to know:
Understanding the neurobiology of migraine helps patients engage with clinicians and lifestyle changes, especially if previous treatments were unsuccessful. This improves the chances of successfully managing their migraines.
Our correspondent’s highlights from the symposium are meant as a fair representation of the scientific content presented. The views and opinions expressed on this page do not necessarily reflect those of Lundbeck.
1. CGRP Forum. Unmet needs in migraine prevention.
2. Linde M et al. Eur J Neurol 2012;19:703-11
3. Coppola G, et al. J Headache Pain 2013;14(1):65.
4. Schwedt T, et al. Headache 2015;55(6):762-77.
5. Schulte L, et al. Neurology 2017;88(21):2011-6.
6. Domínguez C, et al. Neurology 2019;92(10):e1076-85.
7. van Dongen R, et al. Cephalalgia 2017;37(1):49-63.
8. Cernuda-Morollón E, et al. Neurology 2013;81(14):1191-6.
9. Sintas C, et al. J Pain 2016;18(4):366-75.
10. Perry C, et al. Ann Neurol 2017;79(6):1000-13.
11. Bigal M and Lipton R. Headache 2006;46(9):1334-43.
12. The Brainstorm Consortium. Science 2018;360(6395):eaap8757.
13. Key F, et al. PLoS Genet 2018;14(5):e1007298.
14. Leao A. J Neurophysiol 1944;7(6):359-90.
15. Weiller C, et al. Nat Med 1995;1(7):658-60.
16. Burstein R, et al. Brain 2000;123(8):1703-9.