
Choose a channel
Check out the different Progress in Mind content channels.

Progress in Mind
More than 50% of people with first-episode psychosis (FEP) have comorbid substance use disorder (SUD).1,2 Research illustrates that the diagnosis of a comorbid SUD is linked to poor adherence to medication, poor functional outcome and poor symptomatic outcome in FEP patients.1 A number of randomized controlled trials (RCTs) and cohort studies show that treatment with long-acting injectable antipsychotics (LAI-AP) can effectively reduce the number of relapses and hospitalizations in patients with psychosis;3-6 however, few of these studies were conducted in patients with SUD. Results from a naturalistic retrospective study show that results in patients with FEP can be extrapolated to those with FEP-SUD.
A naturalistic, longitudinal descriptive prospective retrospective study was conducted to examine the effects of treatment with LAI-AP in people with FEP and SUD. The study included 237 adults admitted to the Institut Universitaire en Santé Mentale de Montréal (IUSMM) with untreated psychotic illness or previous AP treatment for <12 months, and SUD score >2 on the Drug Use Scale (DUS) or the Alcohol Use Scale (AUS).
Patients were divided into groups according to whether they received LAI-AP as first-line treatment (LAI-AP-first) or oral antipsychotics (OAP) as first-line treatment (OAP-first). Groups were further divided depending on whether they continued on LAI-AP throughout the study (LAI-AP-only), continued on OAP throughout the study (AOP-only), or whether they switched from LAI-AP to OAP (LAI-AP-first-both) or vice versa (OAP-first-both). Patients were initially followed for 3 years.
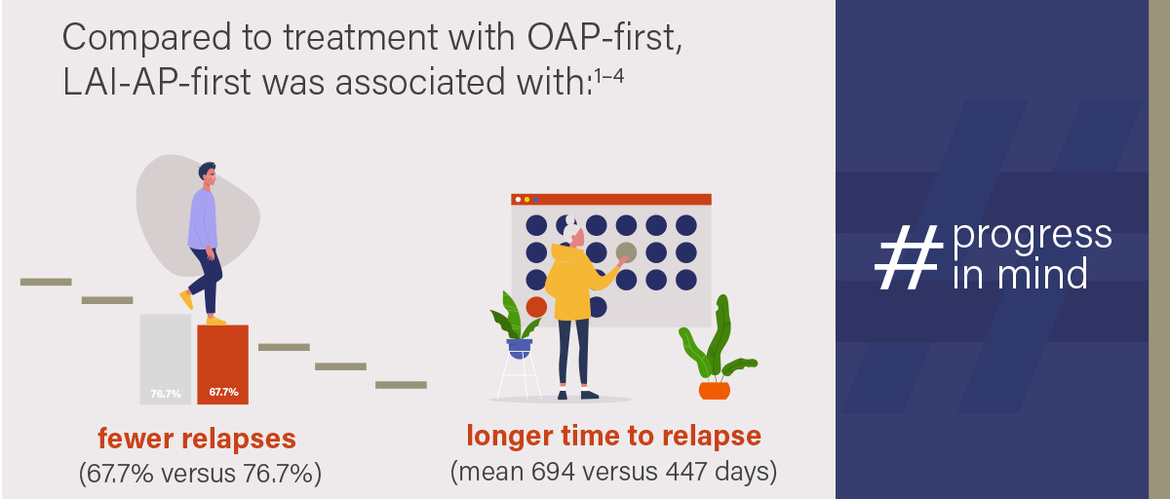
Compared to OAP-first, LAI-AP-first was associated with fewer relapses (67.7% vs. 76.7%) and significantly longer time to relapse (mean 694 vs. 447 days).
Prior to admission, significantly fewer patients receiving LAI-AP-first had financial autonomy compared to those receiving OAP-first (32.3% versus 64.5%). Homelessness prior to admission (38.7% versus 20.0%) and higher PANSS general symptom score at admission (39.5 versus 34.8) were also significantly higher in the LAI-AP-first group.
Compared to OAP-first, LAI-AP-first was associated with fewer relapses (67.7% vs. 76.7%) and significantly longer time to relapse (mean 694 vs. 447 days). There was a trend towards reduced rehospitalization (48.4% vs. 57.3%) and increased hospital-free survival time (813 vs. 619 days) among patients receiving LAI-AP-first; however, results were not significant.
Levels of premorbid functioning prior to admission were greatest among patients receiving OAP-only, slightly lower in LAI-AP/OAP-first-both groups, and even lower in patients receiving LAI-AP-only. The highest percentage of schizophrenia spectrum disorder (88.2%) was observed in the LAI-AP-only group. Despite relatively high proportions of patients with financial autonomy and employment at admission, OAP-first-both patients were younger, with lower levels of education than other groups.
LAI-AP should be offered as first-line treatment to all patients with FEP-SUD, but especially those with factors predicting poor prognosis
Psychotic relapse was significantly higher in the OAP-first-both group (92.9%) than in other groups (70.6% for LAI-AP-only patients, 65.3% for OAP-only patients, and 64.3% for LAI-AP-first-both patients). Relapse-free survival was also significantly worse in the OAP-first both group (352 days versus 703, 527, and 681 days, respectively). Overall, 83.5% of the OAP-first-both group were rehospitalized at least once, compared to 52% of the LAI-AP-first-both patients, 38.9% of the OAP-only patients, and 42.9% of the LAI-AP-first-both group). Hospitalization-free survival was also significantly shorter for the OAP-first-both group (436 days versus 797, 772, and 825 days, respectively).
Overall, results suggest that LAI-AP protects against relapses and rehospitalization in people with FEP-SUD. LAI-AP should therefore be offered as first-line treatment to all patients with FEP-SUD, but especially those with factors predicting poor prognosis, such as low levels of education, schizophrenia, and young age at admission (even if they have good premorbid vocational status).
The study will be continued for a further 2 years to see whether the benefits of first-line treatment with LAI-AP persist over time.
Our correspondent’s highlights from the symposium are meant as a fair representation of the scientific content presented. The views and opinions expressed on this page do not necessarily reflect those of Lundbeck.