
Choose a channel
Check out the different Progress in Mind content channels.

Progress in Mind
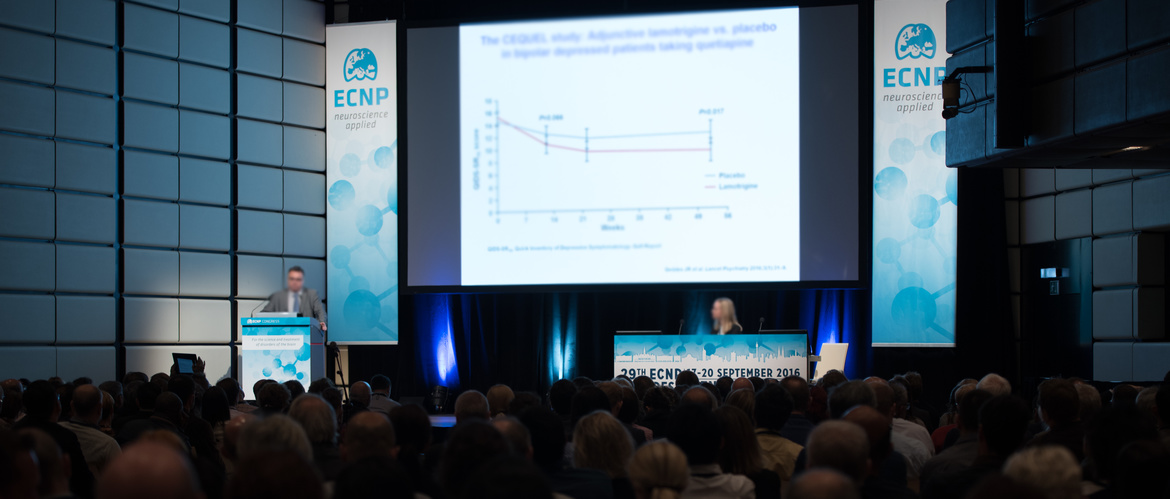
Attempts to treat and manage bipolar disorder (BD) predate current BD definitions and many of the treatments still used in contemporary management found their way into use empirically rather than by design. This makes for an interesting history and evidence-base for practitioners and for researchers. At an ECNP 2016 Educational Update Session, delegates heard how the past continues to inform the future, and were updated on new data and research activities that are starting to change concepts and approaches to BD management.
Treatment of bipolar disorder (BD) has had a major focus on the management of mania and the control of severe symptoms such as agitation, psychotic symptoms and behavioral disinhibition. Professor Eduard Vieta, Professor of Psychiatry at the University of Barcelona, Spain said that today there is good agreement on how to treat mania and agitation effectively, humanely and in a patient-friendly manner, adding that current treatment of mania follows a more ambitious paradigm that in the past.
Contemporary goals include helping patients reach remission – a state in which there are fewer subclinical or residual symptoms that could hamper functional recovery – and preventing mania relapses.
Professor Vieta said however, that attempts at mania management must try to avoid ‘switching patients to the opposite pole’ where they experience the depressive symptoms of BD. In particular, he highlighted that BD treatment guidelines emphasize reducing the risk of suicidal behaviour in BD depression as a crucial goal. Turning to how practitioners should look to manage depression in BD, Professor Vieta described the International Society for Bipolar Disorders (ISBD) Task Force position on the role and use of antidepressant treatments in BD. The ISBD do not recommend antidepressant monotherapy and suggest avoiding this class of drugs in rapidly cycling patients.
He said that current guidance is that clinicians should combine antidepressants with mood stabilizers or antipsychotic agents when seeking to manage depression in BD – noting that the definition of depression in BD follows that for the definition of major depressive disorder (MDD) in current psychiatric disease criteria.
In terms of recommendations for clinical practice, Professor Vieta said he considers that the current British Association for Psychopharmacology (BAP) guidelines capture the evidence-base well and make good recommendations that support the use of antidepressants in patient management. He added that all treatment decisions should be based on the predominant polarity of a patient’s BD. This means aiming for prevention of depression in maintenance treatment of bipolar II patients and prevention of both mania and depression in bipolar I patients. According to Professor Vieta, predominant polarity is both a valid prognostic parameter and a guide for therapeutic decisions. He added that staging of BD is also important when making clinical decisions.
But that doesn’t mean to say that choosing drug treatments for BD is easy. Professor Vieta reminded delegates that treatments used as mood stabilizers come from a wide range of different drug classes and vary greatly in their mechanism of action, efficacy and safety profiles. He then showed a graphic, depicting in sliding linear scale, the predominant activity of different mood stabilizers used in BD – where treatments were assessed by an equation weighing their ‘polarity’ according to their relative anti-manic or anti-depressant effects – an equation based on number needed to treat (NNT) analyses and NNT prevention of depression : NNT prevention of mania. The graphic showed that the majority of drugs used in BD patient care fall largely on the mania side of the scale, with lithium lying between the extremes and very few treatments falling on the side of the scale for predominantly antidepressant activity.
Professor Vieta also touched on the role and the study of psychoeducation and psychosocial interventions in BD – measures which may be effective in early stages of BD and which can be supported by new remote technologies such as patient apps and data collecting devices.
Our correspondent’s highlights from the symposium are meant as a fair representation of the scientific content presented. The views and opinions expressed on this page do not necessarily reflect those of Lundbeck.