
Choose a channel
Check out the different Progress in Mind content channels.

Progress in Mind
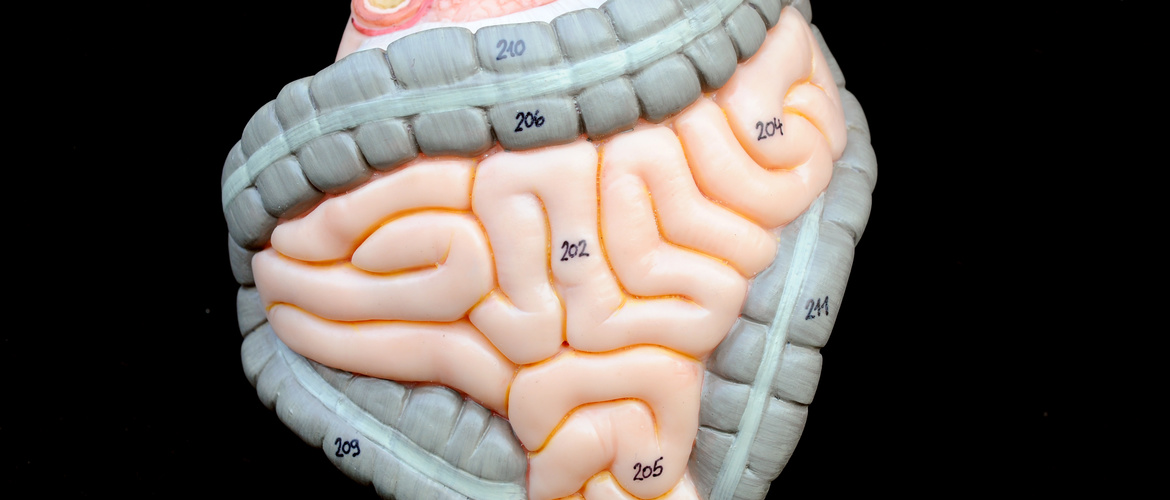
The idea that Parkinson’s Disease begins with alpha-synuclein pathology in the gut which then spreads centrally via the vagal nerve is supported by a growing body of circumstantial evidence. But there are missing pieces in this puzzle.
Perhaps prophetically, James Parkinson envisaged a disordered state of the bowels as a potential precursor to the disease. So it was entirely appropriate that the conference James Parkinson – An Essay on the Shaking Palsy 1817: A Celebration of 200 Years of Progress, organised by the International Parkinson and Movement Disorder Society, included a presentation by Oscar Gershanik, of the Hospital Universitario Favaloro Foundation, Buenos Aires, Argentina, which provided the latest views on whether the disease begins in the gut.
There is strong evidence from mutations of the PARK1 gene that alpha-synuclein is intimately involved in the pathogenesis of PD.1 Currently, it seems that misfolded alpha-synuclein is the specific culprit.2
Alpha-synuclein is widely distributed in the body, and not all forms are neurotoxic. But the oligomeric fibrillar aggregates are – interfering, among other things, with synaptic function, dopamine transport and protein degradation. Moreover, they could form the template for the aggregation of endogenous alpha-synuclein.
For the bowel to brain hypothesis to be true, there must be evidence of alpha-synuclein propagation, and there must be evidence that the alpha-synuclein in brain regions central to Parkinson’s Disease symptoms originates in the gut.
Host to graft transmission suggests self propagating, prion-like spread of α-synuclein
Transplanting the microbiota from PD patients into mice worsened their motor symptoms
Parkinson himself noted the link between PD and prior constipation, and evidence that bowel dysfunction is part of the non-motor prodrome has generally been supported.
Braak and Tredici are among those most associated with the theory that Parkinson’s Disease originates in the enteric nervous system and from there spreads in a prion-like fashion to the dorsal motor nucleus of the vagal nerve in the lower brainstem and thence to the midbrain, forebrain and cortex.7
Alpha-synuclein is physiologically excreted by enteric neurons into the lumen of the intestine. In mice, this is increased by enterotoxins. Sampson and colleagues recently reported the remarkable finding that transplanting the microbiota from PD patients – but not from healthy controls – into mice that overexpress alpha-synuclein worsened motor symptoms.8 This contributed to a growing body of evidence that gut bacteria modulate movement disorders in mice and could be a risk factor for PD.
The work of Claudio Ruffman and others in Oxford, UK, suggests that the density of alpha-synuclein staining in biopsies of colonic mucosa is greater in PD patients than in healthy controls. Novel techniques are being developed in an effort to show that the protein is present in misfolded, oligomeric or fibrillar forms. But there is indeed Lewy body pathology in the enteric nervous system.
PD is associated with increased interstitial permeability of the gut. And there are experimental studies of vagal nerve spread up to the DMV and into the brain. Alpha-synuclein immunoreactivity studies on post mortem brain provide evidence of the caudo-rostral spread of pathology.
So we have a chain of events that runs something like this: inflammation in the gut produces an immune response that increases interstitial permeability. As part of the host response, there is aggregation of alpha-synuclein that spreads along the vagal nerve and into the brain.
That said, there is only one clinical study that supports the suggested route of transmission. Based on access to Danish registries, Svensson et al in 2015 reported that truncal vagotomy but not superselective vagotomy was associated with a decreased risk of developing PD.9 But that finding has not so far been replicated.
And there are several caveats. First, the reporting of constipation in retrospective studies may be confounded by recall bias. Secondly, when it comes to alpha-synuclein in the enteric system, established assay techniques do not distinguish between pathogenic and non-pathogenic forms of the protein: we need a stain that is specific for pathogenic forms.
Thirdly, some publications show colonic alpha-synuclein staining in controls as well as PD patients. Fourth, Braak’s ideas of the systematic spread of alpha-synuclein pathology are not uniformly supported by histological data. And, finally, many pieces in the puzzle are still missing: in particular, we need longitudinal studies in man demonstrating that the pathology does actually spread from gut to brain.
Our correspondent’s highlights from the symposium are meant as a fair representation of the scientific content presented. The views and opinions expressed on this page do not necessarily reflect those of Lundbeck.