
Choose a channel
Check out the different Progress in Mind content channels.

Progress in Mind
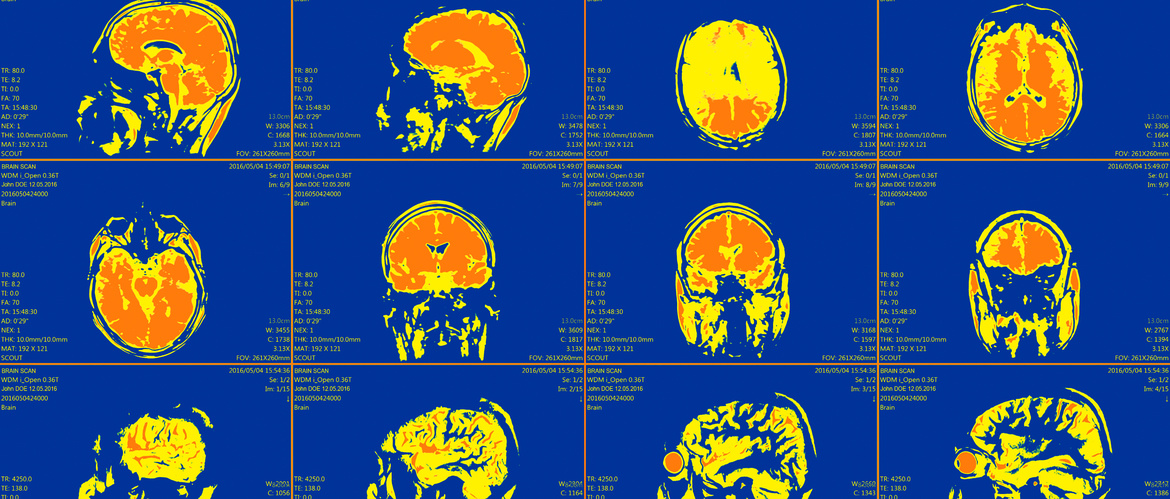
Predicting disease course and predicting response to therapy – including the probability that a person at high risk will transition to psychosis – were areas of clinical priority identified in the brainstorming session on neuroimaging. When it comes to the use of advanced imaging techniques in everyday practice, we are still far from where we want to be. But there are pointers along the way.
If a person with severe mental illness comes to the clinic, we probably do not need a brain scan to reach a diagnosis. But – in an ideal world – it would be very helpful when talking to someone with their first episode of psychosis, and to their relatives, if we knew whether or not their disease was likely to take a relatively benign course.
That might be important enough information to justify the expense of a scan – if we had a reliable imaging biomarker.
Effort should be put into machine learning algorithms relevant to predicting treatment response
In a patient with major depression, we would appreciate to be able to see after a week or so whether the same patient was showing signs of responding to the prescribed treatment.
Catherine Harmer (University of Oxford, UK) mentioned preliminary evidence from neuroimaging which indicated that changes in processing networks when patients are engaged in emotion recognition tasks seem predictive of later symptomatic response to an antidepressant.1
Even if that finding can be replicated, we would still need to know whether an imaging-guided drug changing strategy produced better long-term clinical outcome, Professor Harmer cautioned. But we can imagine that it might.
Recent work shows that people with early schizophrenia and those at high clinical risk of developing the disease have a common functional MRI feature which sets them apart from healthy controls. In this case, it is significantly reduced activation in the bilateral dorsal anterior cingulate and right inferior frontal cortex.2
That interesting observation relates to our understanding of cognitive control deficits in schizophrenia. But we do not know how specific that deficit is; nor whether its presence helps us predict which high-risk individuals are at imminent danger of transition to psychosis.
A recent multimodal neuroimaging study finds a correlation between GABA levels in the medial prefrontal cortex and blood flow in the hippocampus of people at ultra-high risk of psychosis, with differences between those who went on to develop a psychotic disorder over the next two years and those who did not.3 But again, while important, there are no immediate implications for clinical practice.
Exciting MRI and PET findings have been noted, however, the challenge remains as to how these are translated into the clinic
We have exciting MRI and PET findings, but the challenge is to translate them into the clinic, Ole Andreassen (University of Oslo, Norway) told the session.
A brief review of the literature conducted by Carles Soriano-Mas (Bellvitge Biomedical Research Institute Barcelona, Spain) revealed that the largest area of interest has been imaging in schizophrenia, particularly using MRI to map functional connections when patients are engaged in a relevant task, or voxel-based morphometry of regional brain volumes.
The session also considered the potential of imaging in “population neuroscience”, of the kind that might be achieved in large cohort studies such as the UK Biobank.4 But the overall view was that the relative rarity of serious mental illness meant that this should not at the moment be a focus of research.
We are some distance from being able to think of imaging in population screening
We are some distance from being able to think of imaging in population screening. And psychiatrists are not in a position analogous to that of neurologists, who are actively considering whether imaging evidence of amyloid or Tau in the brain should be considered a defining characteristic of Alzheimer’s Disease even in the absence of cognitive symptoms.